LARYNGECTOMY.NET
The hospitalisation and the return home after total laryngectomy
Hospitalisation
The hospitalisation starts the day before the surgery. Since a laryngectomy is a rather long operation (at least 4h), it is often positioned at the start of the surgical schedule.

The patient returns to the hospitalisation department with several Redon drains (at least 2), a urinary catheter, a naso-gastric tube, and one or two surgical approaches. Therefore, the first 2 to 3 days following surgery are a rest period, where the patient remains in bed, and where the drains, catheters and infusion lines are removed one by one. Only the naso-gastric tube is left in position.

After the 3rd day, the patient is rested, the pain controlled and the drains removed. The patient is allowed to leave the bed. The therapeutic education begins. The patient will be taught the emergency procedures, tracheotomy care and means of communication during individual workshops. This second period usually lasts until the 10th day.

At the end of this second 10-day period food is progressively introduced, as long as the wound healing is doing well, and that there is no pharyngostoma. If feeding takes place properly, the naso-gastric tube is removed, and the patient goes home.

The exception to this re-introduction of food at 10d rule are patients who had received pre-operative radiation therapy. In that case, the wound healing is longer, and feeding is only resumed 3 weeks after the surgery. In such cases, the patient is still released on the 10th day, but with a nasogastric tube and with instructions forbidding eating by the mouth. He/she is hospitalised again for feeding at about the 3rd week post-operative.
The return home

The return home usually takes place at about the 10th day.
The patient is given the following prescriptions:
- a prescription for equipment for the care of the tracheostoma orifice
- a prescription for nursing visits for the care of the tracheostoma
- a prescription for suction apparatus and disposable suction tubes
- a prescription with the usual treatments, and analgesics
- a prescription for speech re-education in oro- or tracheo-oesophageal voice, depending on whether there is a phonatory prosthesis or not
- a prescription for an air humidifier, if the patient has dry secretions, with formation of mucous plugs
- a prescription for the care of the scar and removal of staples if they were not removed before discharge
- the prescriptions for the NGT equipment and feed if it was not removed

Concerning the tracheostoma, it must be calibrated by a cannula for several months. The cannula is only there for calibration and can therefore be removed without worrying to examine the patient or for treatments. It is a simple and supple cannula (Larytube).
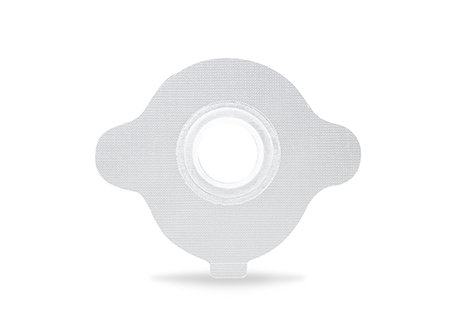
Once this period is over, the patient will be able to place a specific adhesive tape around the tracheostoma, in order to attach the different equipment listed below (these elements are also adapted around the cannula).
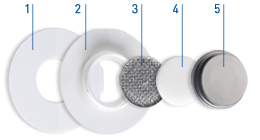
The most important of the elements adapted on the adhesive or cannula is the Heat and Moisture Exchanger, called HME. It is a filter that allows humidifying and heating the air, to reduce the pulmonary inflammatory reaction secondary to dry, cold and unfiltered air.

There are also specific tips for the shower, for free-hands speech, or for other everyday life situations.