LARYNGECTOMY.NET
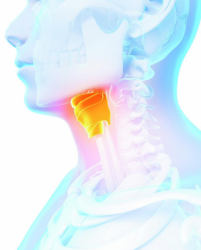
Laryngectomy: definitions and consequences
A total laryngectomy is a mutilating surgery performed within the framework of an advanced cancer of the larynx.
Total laryngectomy is the resection of the larynx and possibly of its annexes, it may be accompanied of a lymph node dissection, which is often bilateral. This surgery lasts between 4 to 6 hours.
It separates the respiratory and digestive tracts. The surgeon connects the trachea to the skin, the orifice thus formed is called a tracheostoma, this allows preserving the passage of air into the lungs, and the pharyngeal sutures restore the tightness of the digestive tract.
The patient will breath in a definitive manner through the orifice of the tracheostoma.
This surgery thus results in a definitive and irreversible modification of the corporal and functional image of the patient: tracheostomy and loss of original voice.
The consequences of the total laryngectomy are diverse.
It separates the respiratory and digestive system. The tracheostomy orifice is final.
– Laryngeal speech is lost. The patient loses his/her original voice and will have to learn to speak again thanks to speech therapy. Vocal rehabilitation will take place once the doctor gives the green light after full healing of the wound. (link to speech pathologist tab)
Before that, other means of communication must be used such as writing on a pad, an erasable slate, whispering, etc.
– Oronasal breathing no longer exists. The person breathes solely through the tracheostomy orifice. The upper aerodigestive tracts no longer fulfil their mission, filtering, humidifying and warming the air. There is also a loss of smell.
– Certain closed glottis efforts can no longer be accomplished (e.g.: defecation, sexual intercourse in men, etc.). Breathing is modified, therefore it will be necessary to adapt these efforts to avoid running out of breath.
– Swallowing is not modified, however there is a potential risk of choking in the case of a phonatory implant.
– Feeding modifications. A nasogastric tube is used for at least the first 10 days post-operative to ensure good wound healing. Afterwards, the diet will be adjusted in terms of textures to return to a normal diet. Alcohol should be avoided as much as possible.
– It is impossible to blow the nose by exhaling air through the nose.
– Besides the functional and physiological consequences, there are obviously psychological consequences. This surgery generates a modification of the body image.
This is why it is essential to support the patient and his/her family from the announcement of the cancer and the surgery up to the return home and afterwards.