LARYNGECTOMY.NET
The care of laryngectomised patient
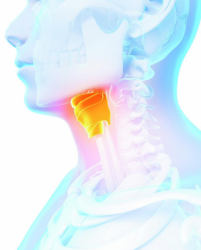
Tracheostoma care
They must be performed every day. Initially, a daily visit by the RN is required to support the patient and up to the end of the healing.
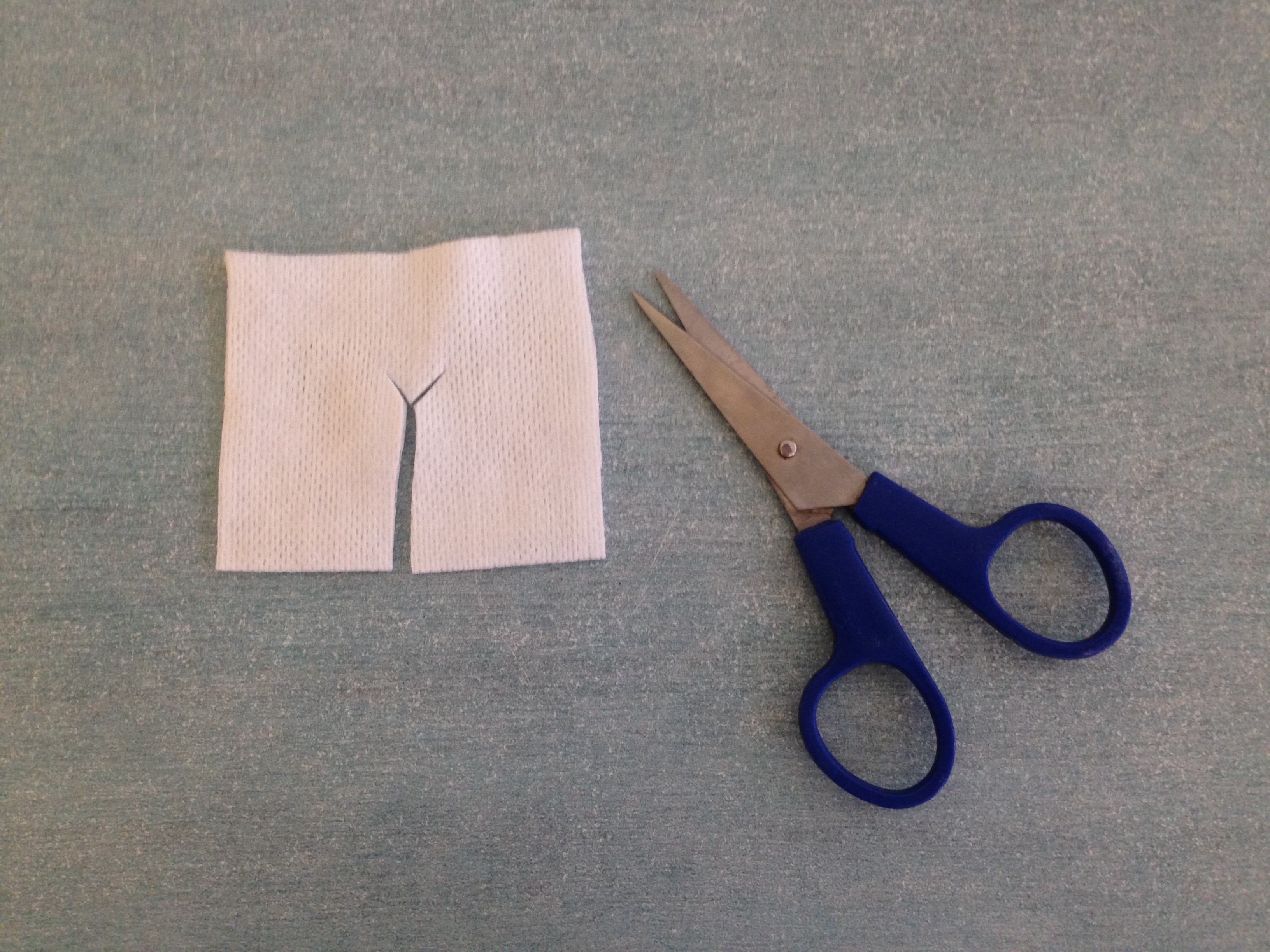
It is important to note that the cannula may be safely removed, since the trachea is connected to the skin there is no risk of the tracheostoma closing. The cannula must be removed and cleaned with clean water using the brush. The tracheostomy orifice is then cleaned with gauze compresses and saline solution. The cannula is re-introduced, a lubricant may be used to facilitate the insertion. The chord is put back and a compress cut in Y (or a specific compress) is inserted between the cannula and skin. It is important to examine the appearance of the orifice (inflammation, redness, pain, abnormal discharge, etc.) in which case the surgeon must be informed.
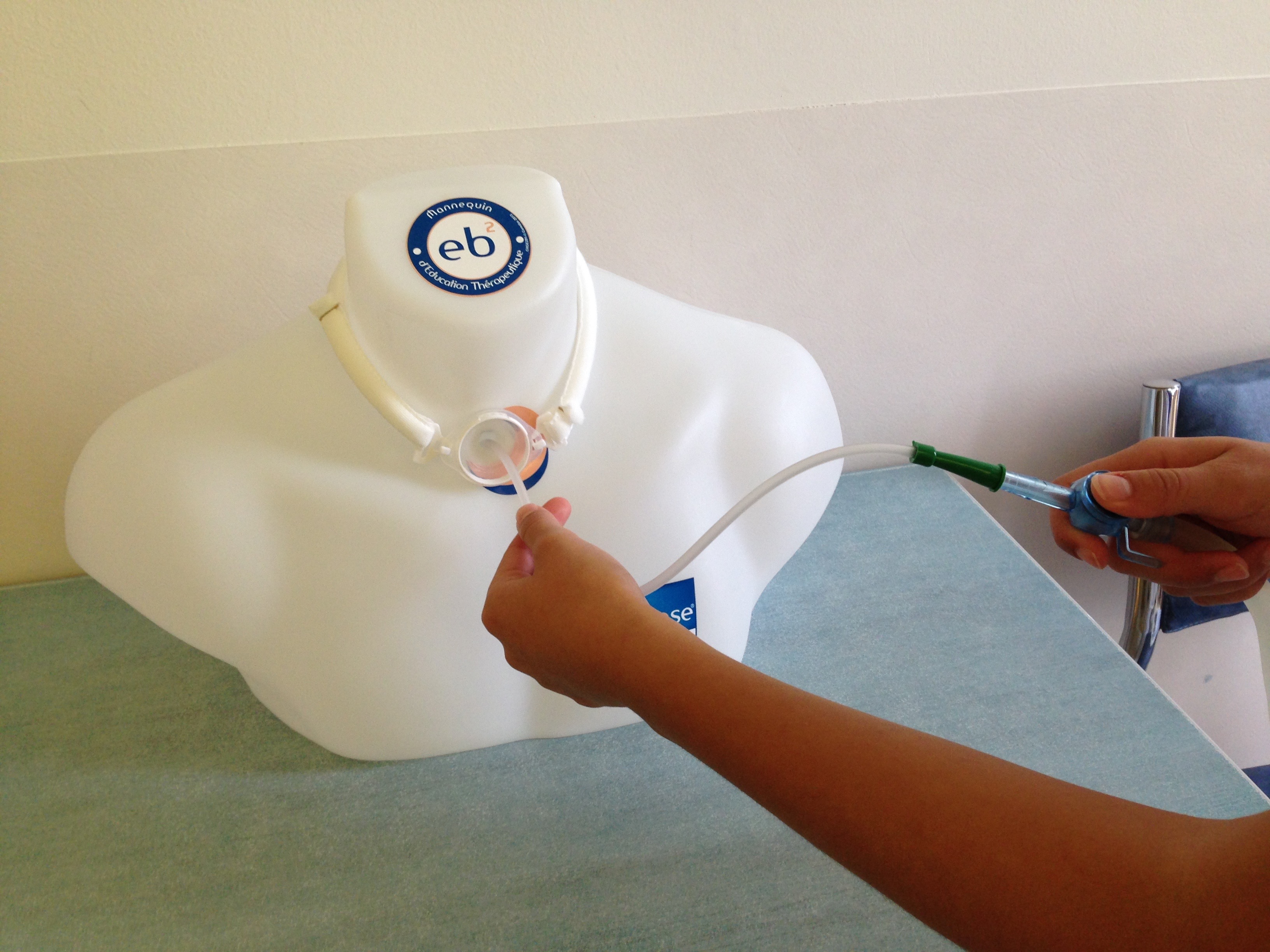
Tracheal suctioning
They are performed if necessary. The catheter is fitted on the suction system. The suction device is turned. The catheter is introduced at approximately 5cm and should not be lowered any further into the cannula to prevent any irritation. The catheter is then drawn up and removed while suctioning and rotating the catheter. Verify that the airways are cleared and repeat if necessary. Finish by rinsing the catheter with the rinse bottle. It is important to verify the appearance of the secretions (fluidity, colour, odour) because there may be an infection indicator.
Emergency situations
Different problems may arise with a laryngectomised patient.
Respiratory distress related to a mucous plug. Since the air cannot be humidified and warmed by the nose, a plug is created by the drying of tracheal secretions and provoke breathing difficulties with a sensation of suffocation. It is therefore important that the patient uses sprays and/or air humidifiers.
Bleeding may occur. It is important to differentiate between irritation bleeding and a haemorrhage. Irritation bleeding may be limited by the use of a spray.
In fact, it is possible that a major neck vessel (carotid) rupture occurs. It is a life-threatening emergency, apply compression and call the Mobile emergency unit for a rapid transfer of the patient to the hospital.
For patients with a phonatory implant, there is a risk of leakage. The phonatory implant is a device that transports air from the trachea to the oesophagus when the tracheostoma is blocked with a finger or by the tracheal valve (see speech therapy tab). This implant may leak causing the passage of liquid from the oesophagus to the trachea and provoke repeated coughing. It is important to inform the surgeon for replacing the implant and tell the patient to stop oral intake until then.
Fistula can also occur, resulting an abnormal passage of liquid towards the oesophagus or creating holes in the skin orifice. Inform the surgeon on discovery.
Speech with the prosthesis:
Risk of leakage with the prosthesis:
Feeding
There are several configurations with respect to feeding.
The patient may be discharged with a nasogastric tube (NST). In such cases, there daily care consists in changing the adhesive plaster on the nose. Verify that the tube is properly placed with respect to the mark given on hospital discharge. Skin monitoring, verify that the tube does not cause eschars in the nasal wings.
Sometimes the patient has a gastrostomy catheter. In such cases, local betadine care will be applied over the first 15 days of insertion of the catheter, and then the care is performed during the cleansing of the patient with soap and water. If the insertion of the gastrostosmy is earlier, verify the skin condition (pain, redness, discharge, bud).
It is important to monitor the nutrition intake via the tube. A service provider is in charge of feeding within the framework of the catheters with respect to the equipment, however often there is monitoring by a dietician. Do not hesitate to contact their department or hospital if you have any questions.
The last case is that when the patient is discharged from hospital after resuming feeding. Verify that the patient has sufficient oral intake using a diet log, monitoring the weight, and that the food is suitable in terms of the texture.